
In this article, we will consider the main types of foot fungus.
All fungal infections are collectively called ringworm. Experts divide them into two main categories - onychomycosis and dermatomycosis. In the first case, microorganisms penetrate under the nail; in the second, the skin is affected. Furthermore, absolutely all types of foot fungus are classified taking into account the causative agent of the disease and the main symptoms.

main types
First, the type of fungus that affects the legs depends on the causative agent of the disease. Pathogenic microorganisms are divided into several groups: dermatophytes, yeasts and fungi. They are capable of causing common injuries such as:
- Onychomycosis;
- Candidiasis;
- Epidermophytosis;
- Rubrophytia.
The latter is the general name of a group of pathologies in which the feet are affected. All diseases are also divided into groups based on clinical manifestations: membrane, moccasin-like, vesicular.
We will consider the types of foot fungus, photos and treatment by alternative methods below.
rubrophytia
The second name of this disease is rubromycosis. It is distinguished by overcrowded blood vessels, dryness and severe desquamation. The pathology develops very slowly and almost imperceptibly for a person who has contracted an infection.
Blister-shaped foot fungus is very unpleasant.
The first signs are itching and desquamation, which become noticeable in the more advanced stages of the disease. Nail damage also occurs at this stage. Externally, the disease is manifested by the appearance of blisters, crusts, plaques, pustules, located across the surface of the sole of the foot. When a large number of plaques and blisters appear, the person begins to experience painful sensations when walking.

Determining the type of foot fungus (photo) plays a key role in the treatment. Before prescribing therapy for rubrophytosis, it is necessary to perform microscopy and study the clinical picture. The elimination of lesions is carried out with exfoliating agents (keratolytics). Most of them are salicylic acid-based ointments and creams. Therapy is often complex. Alongside external agents, antifungal agents are prescribed.
If the illness is severe, you should start taking medication in pill form. Nail blade injuries are treated by removing them with emollients.
This type of foot fungus (see photo above) is characterized by a high degree of infectivity. Just tap the things that the carrier of the infection uses. The likelihood of infection is often increased if a person suffers from excessive sweating, has a weakened immune system, and any damage to the feet.
The causative agent of the disease is the fungus Tr. Mentagrophytesvar. It is capable of penetrating the granular layers and stratum corneum of the skin, spreading and causing severe reactions of one allergic type and another:
- pain when walking, burning and itching;
- deformation and yellowing of the nails;
- the appearance of crusts, scales, painful cracks;
- skin erosion (maceration);
- the appearance of pustules, edema;
- vesicle rash with a dense crust.

The diagnosis of this type of foot fungus consists of studying the external signs and the clinical picture. If the causative agent of the condition is not obvious, clinical research may be needed, for example, examining the scrape under a microscope.
The therapy of rubrophytosis in the acute form involves the use of drugs based on 0. 25% silver nitrate, 10% calcium and 1% meta-dihydroxybenzene. If allergic reactions occur, antihistamines should be used. The choice of antifungal agent depends entirely on the clinical course of the disease and the individual characteristics of the patient's body.
What other types of foot fungus are there?
Candidiasis of the foot
This type of fungus occurs in patients much less frequently than epidermophytosis or rubromycosis. The pathology occurs under the influence of a fungus of the Candida genus. These microorganisms live in each person's body, however, they are considered conditionally pathogenic. That is, they do not pose a threat in small amounts, but their rapid multiplication can cause unpleasant symptoms and consequences. The uncontrolled reproduction of the fungus begins if there is a decrease in immunity during hypothermia, by overwork or frequent stress. External factors include:
- to wear, particularly in summer, uncomfortable shoes;
- injuries received at home or at work;
- constant maceration of the skin of the feet (exfoliation of the skin by prolonged exposure to water).
There are two types of foot candidiasis: hyperkeratotic and vesicular-pustular. The first form of candidiasis is characterized by thickening of the stratum corneum. In it, very wide furrows begin to appear, light brown in color, which detach constantly. For diagnostic purposes, exfoliation is performed and the particles in which the Candida fungi are found are later studied.

The viscous-pustular form of candidiasis manifests as hyperemia (overcrowding of blood vessels), pronounced edema, and maceration. Areas of affected skin are covered with pustules and small flat blisters. After the extinction of the inflammatory processes, desquamation occurs. Appointment of therapy is only possible after the exact diagnosis has been determined. The choice of medication for this type of foot fungus with blisters is made individually. Most of the time, systemic and local medications are shown.
onychomycosis
This disease is a type of foot fungus, characterized by a fungal infection of the toenail. You can get infected in public showers, saunas, baths, swimming pools. Scales containing a pathogenic microorganism are easily separated from the nail plate and can remain on unpainted floors, carpets, mats and countertops. High humidity not only allows for survival, but also promotes active reproduction and therefore the risk of infection increases significantly.
In the early stage, the infection penetrates the epidermis of the feet, causing intense itching. To weaken the unpleasant sensations, the person begins to search the infected area, but with that the situation only worsens. The areas of skin affected by the fungus are covered by small scratches and cracks, the microorganisms begin to spread, penetrate under the nail plate, after which they begin to multiply uncontrollably.
Serious illnesses such as diabetes or HIV, impaired blood circulation and nail trauma greatly increase the risk of infection.
Onychomycosis is classified into 3 types:

- Normotrophic. With this type of onychomycosis, a change in nail color from normal to brownish-yellow is observed. The natural shine, shape and thickness of the nails remain unchanged.
- Hypertrophic. There is a final change in the color of the nail, its shine disappears, the shape changes, the thickening develops and partial destruction begins.
- Onycholytic. The color of the affected nail changes to brown, becomes thinner, starts to break. Your gradual separation from the bed begins. In the open part of the nail bed, uneven layers can be observed.
The therapy of this type of fungus on the palms of the hands and feet with topical medications is ineffective because the fungus spores are located under the nails. Before starting treatment, the nail must be removed. This is done with keratolytic drugs, and patches are also used. In some cases, there is the possibility of mechanical removal of the nail: particles from the nail that have died are cut with a file or tweezers. It is important to remember that all instruments used must be sterile.
The combined use of mechanical removal and keratolytic adhesives is the most effective way to remove a diseased nail. From keratolytic agents, you can use a ready-made set, which contains a special ointment, files to scrape the nail, a plaster. After removing the nail plate, you should start taking systemic antimycotics.
It is quite difficult to determine the type of foot fungus in the photo.

Interdigital form (intertriginous)
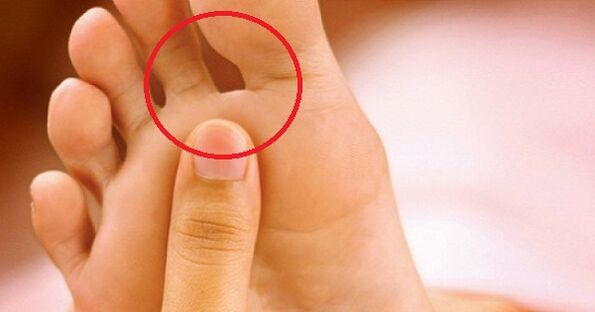
The most common and unpleasant type of pathology is the intertriginous form of fungal infection. Appears quite often in summer, begins to develop between the third and fourth toes. Over time, the lesion spreads to areas between the other fingers.
At first, a small crack, funnel or sore appears in the crease located between the fingers. It is surrounded by diaper rash or slightly greenish scaly skin. Most of the time the damage gets wet, sometimes pus runs off it. The type of extinguished fungus is characterized by pronounced peeling or chalky, as if there were flour on the surface of the finger. A similar impression arises from the large number of affected scales that separate from the skin. There is a slight itching that does not cause severe discomfort.
In the advanced form of the disease, there is delamination of the nails, accentuated thickening, multiple fissures, calluses similar to corneal compaction, and pronounced yellowing.
In very rare cases, a weeping-like illness - an exudative fungus - develops. Its main difference is that the vesicles are spilled into the affected areas - fluid-filled bubbles inside. Therapy must be carried out comprehensively. Antifungal agents are used as topical agents. The advanced form of the disease involves the use of systemic antimycotics. The course of treatment should be continued until the fungus completely disappears.
Squamous-hyperkeratotic form
This type of foot fungus (pictured below) is not very common.

Squamosis is the process of penetration of pathogenic fungi into the skin's outer cells. Hyperkeratosis is the formation of the stratum corneum, resulting in a thickening of the dermis. In this sense, the scaly-hyperkeratotic form of ringworm has several other names, for example, "moccasin fungus" and "athlete's foot".
The squamous-hyperkeratotic type of ringworm is characterized by the following symptoms:
- The sole of the foot is covered with a thick layer of keratinization from the dermis, resulting in the impression that the feet wear moccasins.
- The thickening of the sole of the foot occurs so strongly that it starts to be covered by large, thick calluses.
- Painful cracks appear on the corns.
- The desquamation takes on a mucous type, a pattern on the skin visible to the naked eye.
- An unbearable itching appears.
- Over time, nails begin to thin, break and crumble.
In the treatment of moccasin fungus, first of all, it is very important to remove the stratum corneum from the skin. This is done with foot soap, bandages, salicylic compresses, and ichthyol ointments. Salicylic ointment is used in dosages of up to 10%. Vaseline-based creams, ointments containing lactic acid are effective. If you are unable to perform this task at home, you should seek help from a podiatry center. With the help of a hardware manicure, the specialist will carefully remove the keratinized dermis.
Subsequent treatment for the type of foot fungus will depend on the type of pathogen. It should only be started after an accurate diagnosis has been made. It is not recommended to treat moccasin ringworm without first removing the stratum corneum from the skin - the active components in the drug composition will not be able to penetrate it and reach the focus of infection. As a result, all efforts will be nullified.
Photos of types of foot fungus may not fully reflect all the unpleasant symptoms a person experiences.
Dehydrated form
The vesicular fungus, or as it is also called, dyshydratic mycosis, is the rarest type of disease. Its main manifestation is numerous vesicles combined in conglomerates. Vesicles are vesicles filled with pus or nourishing fluid from within. When the cloudiness of the liquid starts, the vesicles burst, the ulcers remain in place. They begin to fuse into a line, forming sharp scars on the skin. This is due to dryness and peeling of the skin's layers.
About 70% of vesicular fungal infections are accompanied by allergic skin rashes. A variety of bacteria and viruses begin to penetrate ulcers. As a result, the disease becomes mixed and identification of the initial pathogen becomes more difficult. Therefore, you should see a doctor immediately as soon as the primary symptoms appear (pictured): he can quickly identify the type of foot fungus and start therapy.
And this must be done immediately. First of all, before using antimycotics, the acute process must be eliminated. It is best to entrust this task to a specialist: he will be able to gently pierce the vesicles, treat the remaining ulcers with 2% boric acid and scrub with bright green or methylene blue solution.
Treatment of the disease in its neglected form involves the use of corticosteroid ointments. After eliminating the inflammatory process, the use of local antimycotics is recommended. This will suppress the causative agent of the disease.
We continue to consider the names and types of foot fungi.
Deleted form
Ringworm of the erased form is almost invisible, its symptoms are minimal. These include: mild itching, burning, mucous-like desquamation, micro-cracks located in the interdigital areas. If you don't see a specialist when the first signs of the disease appear, the condition can develop into the form of onychomycosis, which is much more difficult to treat. In this case, the detached nail will grow from one to six months.
Treat ringworm in the erased form with local preparations: ointments, creams, foams. They allow you to create a layer on your foot that will protect you from other infections. It is not recommended to wash your feet within 24 hours of applying this medication.
Only in extreme cases can systemic therapy be prescribed. The problem is that these drugs are toxic and negatively affect some internal organs, for example the liver. Therefore, if there is an effect from using local remedies, then it is better not to take pills.
Treating Foot Fungus Types With Alternative Methods
The pathology photos presented in the article in large numbers do not cancel the visit to the doctor.
It's very easy to choose a drug now. However, many people prefer to treat the fungus with folk remedies. We offer several proven recipes:
- Cleaning your feet. The legs are warmed in a basin of hot water, scrubbed thoroughly with washing powder, and treated with a stiff foot brush for five minutes. The foam is rinsed off. Actions are repeated 4-5 times. Then the feet are dried and smeared with cream.
- Celandine Baths. 50 g of herbs are poured with 1, 5 liter of boiling water, heated on fire for 4-5 minutes, cooled. The feet should be kept in warm broth for 30 minutes. Duration of treatment is 14 days.
- Tea tree oil is a powerful antiseptic. It should be rubbed repeatedly on the affected areas.
- You can get rid of itchiness and cracking with heavy cream. She lubricates her legs before going to bed. Duration of therapy is 1 week.
- Sodium bicarbonate. Eliminates burning and itchy skin. The powder is mixed with water to obtain a thick mass. It is applied to the affected areas, wait until it dries and then rinse.
- Calendula. Flowers (50 gr. ) Are poured with boiling water (1: 2), insisted for 30 minutes, filtered. Feet lubricated by infusion at night.

Prophylaxis
The simplest preventive measures will significantly reduce the likelihood of infection. Only personal items should be used, nails should be treated with sterile instruments. When visiting public places such as baths, saunas, swimming pools, beaches, you should wear your own shoes. By the way, try to choose a way that is comfortable and allows your legs to breathe.
You should be concerned about prevention in advance so that you don't have to deal with various types of foot fungus afterwards. The photo shows away from all the options for the development of the disease.















